When it comes to medical marijuana, many consider glaucoma the condition that started it all. However, research has raised several concerns. CannaMD investigates each claim and presents the facts that every glaucoma patient needs to know.
What is glaucoma?
Glaucoma is a group of diseases that damage the optic nerve, a cable that carries visual information from the eye to the brain.
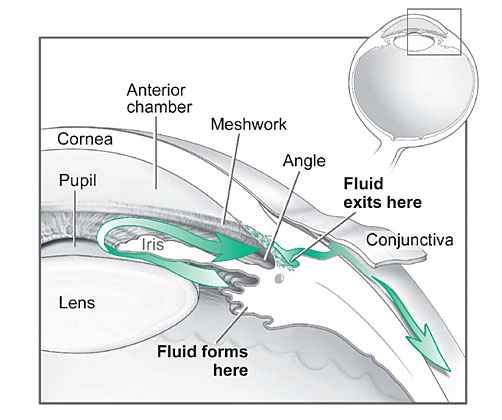
In open-angle glaucoma, the most common form of the disease, fluid passing through the anterior chamber (see diagram, below) drains too slowly, leading to increased eye pressure – or intraocular pressure (IOP). This pressure can damage the optic nerve, leading to vision loss or blindness.
New studies suggest low ocular perfusion pressure (OPP) – the pressure at which blood enters the eye – may also cause glaucoma.
First marijuana and glaucoma studies
In 1971, researchers reported a 25-30% IOP lowering effect of smoking marijuana in a small group of subjects. A 1984 animal study drew similar conclusions:
“These results indicate that chronic administration of [marijuana compounds, cannabinol and cannabigerol] lowers ocular tension considerably.”
While researchers are torn on what causes the IOP lowering effect – some think it’s related to marijuana’s ability to lower blood pressure while others suggest the drug acts on cannabinoid receptors in the eye, decreasing fluid production (instead of directly altering pressure) – one thing is for sure:
Marijuana has been shown to consistently lower IOP approximately 25% in the majority (60-65%) of both glaucoma and non-glaucoma patients. According to the American Glaucoma Society:
“It has been definitively demonstrated, and widely appreciated, that smoking marijuana lowers IOP in both normal individuals and in those with glaucoma, and therefore might be a treatment for glaucoma.”
However, concerns still remain.
Marijuana criticism
The same researchers who linked marijuana’s affect on blood pressure to lowered IOP also suggested its mechanism of action may cause more harm than good. Specifically: they were worried about perfusion (the passage of blood through the circulatory or lymphatic system) to the ciliary body (the part of the eye that controls the shape of the lens and production of the liquid discussed earlier). Less pressure equals less power to move blood, resulting in low OPP.
Lowered blood pressure also means decreased blood flow to the optic nerve – which doctors worry could cause harm.
Lastly, many point to marijuana’s short duration of action (approximately three to four hours), which might require patients to use the medication multiple times throughout the day.
Marijuana defense
As Dr. Farnaz Memarzedah of the University of Southern California’s Doheny Eye Center notes:
“The pathophysiology of primary open-angle glaucoma remains unknown.”
And, while low OPP may be gaining popularity in medical circles (see The American Academy of Ophthalmology’s latest article, The ‘New’ Pressure for Glaucoma Specialists: Ocular Perfusion Arrives), researchers are quick to highlight complexity surrounding the issue. Discussing the 2014 opinion of British researchers Costa et al., a follow-up letter in Acta Ophthalmologica explains:
“For the majority of studies in this field, blood pressure (BP) minus intraocular pressure (IOP) has been used as a simple surrogate measure of OPP. The authors of the review article correctly acknowledge that interpretation of these surrogate measures is problematic and that any crude association observed between OPP and glaucoma may be related solely to the IOP component, given the known strength of IOP as a risk factor for glaucoma.”
Long story short?
Marijuana lowers IOP. And while it may also lower OPP, doctors aren’t sure how and to what extent this effect might impact disease progression. A number of issues – including clarifying relationships between variables – remains to be solved.
For this reason, many ophthalmologists choose to reserve marijuana for end-stage glaucoma. As Dr. Andrew Baisson notes, marijuana can be “very effective” at treating advanced glaucoma symptoms (including pain and nausea).
However, recent research suggests glaucoma may be more of a neurological disorder (like Parkinson’s or Alzheimer’s) than an eye disease – meaning marijuana’s well established, neuroprotective benefits may elevate the treatment in some medical opinions. The American Glaucoma Society adds support:
“An exciting finding in the past decade is the discovery of receptors for the active components of marijuana in the tissues of the eye itself, suggesting that local administration has the possibility of being effective. Furthermore, there is evidence from research in the brain that there may be properties of the cannabinoid components of marijuana that protect nerve cells like those in the optic nerve. This raises the hope that marijuana or related compounds could protect the optic nerve not only through IOP lowering but also through a neuroprotective mechanism.”
For updates on new studies, follow CannaMD on Facebook.
What patients say about marijuana and glaucoma
Long-time glaucoma patient Elvy Mussika has documented her medical marijuana experience in the video, below:
Among her revelations, Mussika notes:
“One of the benefits of using marijuana is that most of us drop all the other drugs that really do a number on our heads and make it difficult for us to stay healthy between our livers, kidneys, and everything else about us. It takes other pills to take care of everything else. I don’t have to deal with that. I did discover marijuana and pretty soon I found that it was the only medicine I ever needed.”
While the jury’s still out on what causes glaucoma (and how exactly marijuana helps), the answer to today’s question is pretty straightforward:
Marijuana is still a good idea for glaucoma – as long as treatment is recommended and supervised by a qualified physician.
If you’re a current glaucoma patient or caregiver, we’d love to hear about your experiences. Please feel free to share thoughts, questions, and stories in the comments section, below!





